Foundations of Dermophthalmology
The Scientific Basis Behind the Skin–Eye Connection
Dermophthalmology is built upon a solid scientific foundation that connects ocular physiology and cutaneous biology through their shared embryological origin — the ectoderm.
From the earliest stages of development, both the eye and the skin arise from the same germ layer, sharing similar cellular structures, immune mechanisms, and microbiological ecosystems.
This anatomical and biological continuity explains why conditions of the skin often reflect on the eyes, and why maintaining eyelid and periocular hygiene is essential not only for comfort and vision, but also for aesthetics and aging prevention.
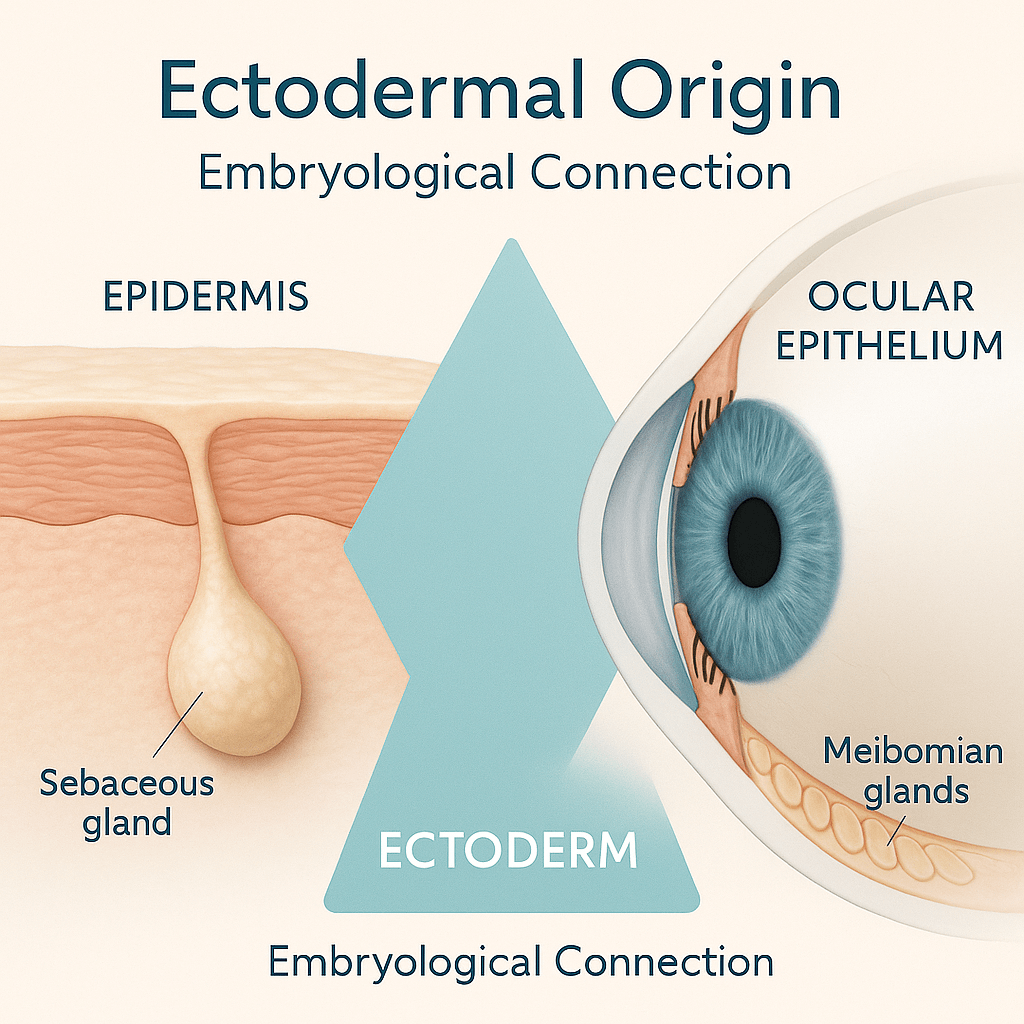
1. Embryological Foundations – The Ectodermal Origin
- Similar barrier and defense mechanisms (tight junctions, lipid layers, immune regulation).
- Parallel sebaceous and glandular structures, such as the meibomian glands in the eyelids and sebaceous glands in the skin.
- Common inflammatory pathways
(IL-1, IL-6, TNF-α) linking ocular surface inflammation and cutaneous dysbiosis.

2. The Meibomian Gland as a Dermatological–Ophthalmic Structure
The meibomian glands are specialized sebaceous glands located in the tarsal plates of the eyelids.
Their lipid secretions (meibum) stabilize the tear film and prevent its evaporation — a process directly influenced by skin health, sebum composition, and microbial balance.
Clinical research confirms that:
- Dysfunction of the glands (MGD) is associated with rosacea, seborrheic dermatitis, psoriasis, and Demodex infestation.
- Chronic inflammation leads to tear film instability, dry eye, and ocular surface aging.
References:
– Nichols KK et al. The International Workshop on Meibomian Gland Dysfunction. Invest Ophthalmol Vis Sci. 2011.
– Liang L et al. Ocular surface microbial communities in meibomian gland dysfunction. PLoS ONE. 2020.

3. Microbiome, Hygiene, and Prevention
Modern studies reveal a dynamic ocular microbiome, similar in complexity to the cutaneous microbiome.
When eyelid hygiene is neglected, biofilms and Demodex mites proliferate, triggering blepharitis and secondary ocular surface inflammation.
Daily hygiene with ophthalmologically specialized mild cleansers, heat therapy, and antimicrobial natural agents (e.g., tea tree oil) — restores balance, reduces inflammation, and supports long-term ocular health.
References:
– Gao YY et al. Detection of Demodex folliculorum in patients with blepharitis. Invest Ophthalmol Vis Sci. 2005.
– Kugadas A, Gadjeva M. The ocular surface microbiome: balancing protection and inflammation. Front Immunol. 2016.

4. From Function to Aesthetics – The Eye as an Organ of Expression
The eyelids and lashes are functional and aesthetic units.
Chronic irritation, inflammation, or gland obstruction not only cause discomfort but also dark circles, puffiness, and loss of lash vitality.
This convergence of science and beauty establishes Dermophthalmology as a discipline of both medical necessity and aesthetic harmony.
References:
– Amador GJ et al. Eye lashes optimize airflow and particle filtration. J R Soc Interface. 2015.
– Osae EA et al. Dysregulation of lipid metabolism in meibomian gland dysfunction. Int J Mol Sci. 2021.
Conclusion
Dermophthalmology is not a theoretical fusion — it is a biological continuum grounded in measurable science.
By understanding and caring for the skin–eye interface, clinicians and researchers can prevent disease, preserve beauty, and redefine the future of ocular and facial health.
